ESBL prediction scores can help get a patient on the most appropriate therapy sooner, even several days before an ESBL has been identified. We recently interviewed Joseph Kohn, Antibiotic Stewardship and Support Team System Coordinator at Prisma Health to learn more about ESBL and gain insights on using an ESBL prediction score in the Firstline app.
Tell us about your role in Antimicrobial Stewardship.
Joseph Kohn: My day to day activities (prior to COVID-19) include: 1) reviewing patients receiving criteria-based or restricted antimicrobials such as the carbapenems, daptomycin, and the newer antimicrobials on the market that target multi-drug resistant organisms, 2) responding to real-time positive blood cultures identified via rapid-diagnostics, 3) assisting with transitions of care for patients with Clostridioides difficile, 4) review of cefepime and piperacillin/tazobactam therapies beyond 72 hours. Since COVID-19, I have also been involved in guideline development, assisting with COVID-19 therapies (remdesivir, tocilizumab, baricitinib, monoclonal antibodies), and medication supply management. As coordinator, I also collect and analyze our antimicrobial utilization (AU) metrics such as days of therapy per 1000 days present, as well as submitting our AU to NHSN to determine our Standardized Antibiotic Administration Ratios (SAARs) for our local facilities. I also work with our Microbiology Lab to develop our annual antibiograms.
Why is it important for antimicrobial stewardship to develop a risk score predicting the probability of bloodstream infections due to extended-spectrum β-lactamase-producing Enterobacteriaceae (ESBLE)?
Joseph Kohn: At first glance, one may think our ESBL Risk Score is a tool to decrease use of carbapenems. Actually, the risk score has assisted in decreasing our utilization of cefepime and piperacillin/tazobactam, which are our most commonly used empiric therapies for gram-negative coverage. Based on our local susceptibilities, it has allowed us to de-escalate to ceftriaxone quicker in many patients. It has also allowed us to escalate to appropriate ESBL coverage several days before an ESBL has been identified, which ultimately has a bigger impact for the patient as they are initiated on the appropriate therapy much sooner.
You co-authored a study on the Clinical Risk Score for Prediction of Extended-Spectrum β-Lactamase-Producing Enterobacteriaceae in Bloodstream Isolates. What outcomes have you seen since using this intervention at Prisma Health?
Joseph Kohn: Our team has been on a mission to transform empirical antimicrobial therapy from a “one size fits all” approach to an evidence-based selection according to each patient’s specific risk of antimicrobial resistance. The ESBL Risk Score along with our other prediction tools provide objective and precise assessment of the risk of infections due to Pseudomonas aeruginosa, ESBL producing and fluoroquinolone-resistant bacteria. Application of these tools has been demonstrated to increase the adequacy of empirical antimicrobial therapy while reducing utilization of broad-spectrum antimicrobial agents.
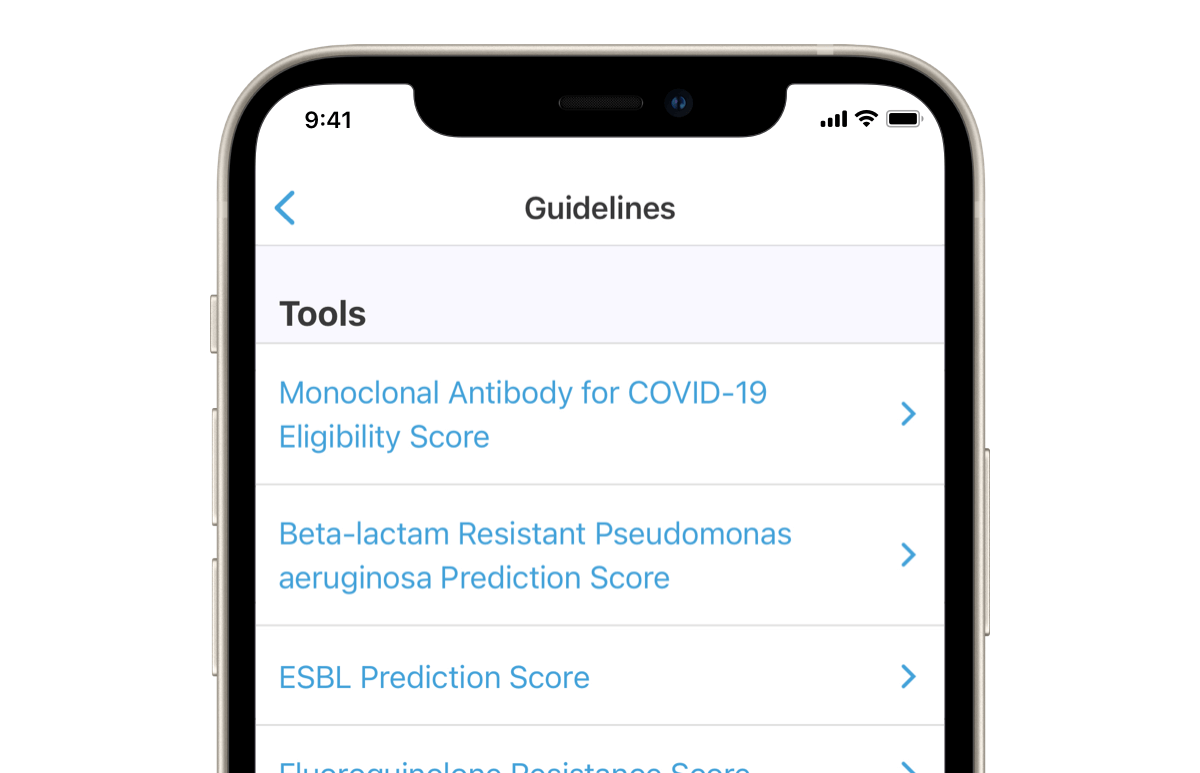
You include the ESBL prediction score in your guidelines in the Firstline app. Looking at the analytics for the app at Prisma Health, it’s been one of the top 5 guidelines accessed this past month, with the majority of use coming from medical students. How does having the ESBL score guideline in Firstline help you to educate your providers on treating bloodstream infections?
Joseph Kohn: The ESBL Prediction Score, along with the Pseudomonas aeruginosa Prediction Score and the Fluoroquinolone Resistance Score, helps us move towards precision or individualized antimicrobial therapy instead of a “one size fits all” approach, which is an important concept to introduce early to the young healthcare providers we work with in our health system.
What kind of questions and feedback do you get from your providers who use this tool?
Joseph Kohn: The feedback has been very positive and has encouraged us to look at opportunities to develop other prediction tools that would benefit our patients, such as a Trimethoprim/Sulfamethoxazole Resistance Score, which is coming soon.
What changes and outcomes have you seen since it’s been so easily accessible to your providers at the point of care in the Firstline app?
Joseph Kohn: Our work over the past few years highlights the successful implementation of an “all-hands-on” antimicrobial stewardship approach - unified vision, leadership support, technological resources, state-of-the-art rapid diagnostics, proactive education, and multidisciplinary collaborative interventions - to optimize antimicrobial use at our healthcare system. This team-based approach improved the quality of empirical antimicrobial therapy in critically-ill patients, reduced antimicrobial utilization of broad-spectrum agents, and improved antimicrobial susceptibilities of predominantly hospital-onset bacteria such as Pseudomonas aeruginosa at our hospitals. Building on the success of prior syndrome-specific interventions and the ease of accessing our locally derived guidelines in the Firstline app, we have been able to take antimicrobial therapy to a new level allowing safe de-escalation of broad-spectrum antimicrobials optimizing patient care. Furthermore, it has allowed our Antimicrobial Stewardship Team to play a major role in Prisma Health’s COVID-19 response while maintaining antimicrobial stewardship activities at a high level despite multiple competing priorities.
What else do you think is important to know about the ESBL Prediction Score in Firstline?
Joseph Kohn:: It is important to understand what is happening locally in terms of microbiology and infections. We have recognized during our most recent COVID-19 surge that we are seeing more and more ESBL infections develop in our community and not within our healthcare systems. Thus, the ESBL Risk Score becomes only a part of the entire patient assessment and escalating therapy is often more appropriate. Also, the ESBL Risk Score will play less of a role for us as we begin utilizing new rapid diagnostics that are capable of identifying ESBL-producing organisms within hours of obtaining blood cultures.
Check out Prisma Health’s guidelines in Firstline
Join Joseph and other ASP leads in the new Firstline Community - a free platform connecting all infectious disease specialists, to share guidelines, learn from each other and spread trusted knowledge.